bringing data science from research to the clinic
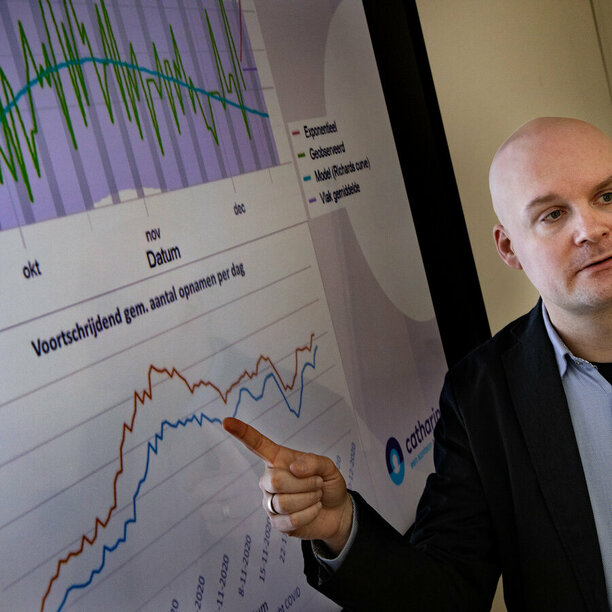
To tackle the problems of bringing data science from research to the clinic, a methodology has been set up to accelerate a process of digital innovation in a specific area of healthcare, in which it is possible to work as one team, consisting of clinical and technical experts from the Catharina Hospital, Philips Research and the Eindhoven University of Technology (TU/e) with expertise ranging from the fields of data science & AI, medicine, IT and business.
Bench to Bedside case studies
Since January 2020 different projects started with 10 experts with weekly working sessions on-site (Catharina Hospital and Philips at the High Tech Campus Eindhoven) and later on digitally. Since then, the team grew and every 6 months new deliverables have been created, tested and validated.
NEWS
Bench-to-Bedside e/MTIC team will highlight power of AI-driven capacity management at the Predictive Analytics World in Healthcare conference US
The research teams have been working on several topics. One of them focused on solutions for detecting and preventing falls using natural language processing (NLP) techniques on doctor and nursing notes within the Electronic Medical Record (EMR), in close collaboration with the geriatric department. Another example covers treatment decision support on post-cardiothoracic surgical patients presenting with ischemia, using patient similarity principles in close collaboration with the anaesthesiology department, cardiology and cardio-surgery experts.
After 6 months, 2 proof of concepts have been developed and successfully presented to a broader team of knowledgeable people in the e/MTIC ecosystem. Next to the tangible results, this pilot shows that working in a multidisciplinary team in a structured way really helps accelerating digital innovation in healthcare. Our 4 main takeaways are:
- In a short period of time, we achieved more together than we are able to do alone.
- Working together on algorithm development within the hospital systems shows the challenges on data management directly at the source. Incorporating these challenges at the beginning of the project, will prevent time-intensive migrations and frustration in a later phase.
- By starting from a relevant clinical need and continuously involving clinicians during the creation of a new tool, the likelihood for acceptance is expected to be much bigger.
- All participants appreciated the contributions of each team member. Their different knowledge and background led to a quicker mutual understanding and increased creativity.
Ideas and comments on new use cases and/or this way of working are welcome for future innovation cycles within the e/MTIC ecosystem. Please send an email to: bench2bedside@emtic.nl.