Novel treatment strategies for an ever-active ageing population
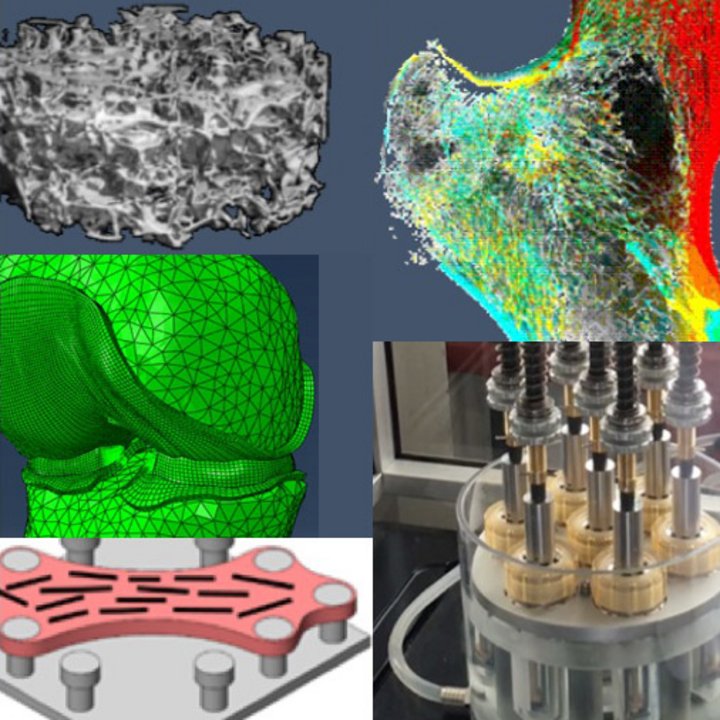
Human cells produce, maintain and adapt musculoskeletal tissues such as bone and cartilage as a response to their biophysical environment, both in health and disease. In our ever-aging population, orthopaedic injuries and degenerative diseases have become more prevalent, with an increasing socioeconomic impact. Current treatment methods with purely synthetic devices may be limited in view of the increasing longevity and high level of activity of modern day humans. The Orthopaedic Biomechanics research group combines engineering and biology to expand our understanding of musculoskeletal tissues and to develop (regenerative) treatment strategies. These are currently applied to bone, articular cartilage, intervertebral disc and tendons/ligaments.
Research Lines
Meet some of our Researchers
Recent Publications
Our most recent peer reviewed publications
-
Penney M. Gilbert,Sandra Hofmann,Huck Hui Ng,Hugo Vankelecom,James M. Wells
Organoids in endocrine and metabolic research
Nature Reviews Endocrinology (2024) -
Jietao Xu,Jana Vecstaudza,Marinus A. Wesdorp,Margot Labberté,Nicole Kops,Manuela Salerno,Joeri Kok,Marina Simon,Marie-Françoise Harmand,Karin Vancíková
Incorporating strontium enriched amorphous calcium phosphate granules in collagen/collagen-magnesium-hydroxyapatite osteochondral scaffolds improves subchondral bone repair
Materials Today Bio (2024) -
Rakia Dhaoui,Saira L. Cazarez,Li Xing,Elmira Baghdadi,Justin T. Mulvey,Nehal S. Idris,Paul J. Hurst,M. Paula Vena,Giuseppe Di Palma,Joseph P. Patterson
3D Visualization of Proteins within Metal–Organic Frameworks via Ferritin-Enabled Electron Microscopy
Advanced Functional Materials (2024) -
Gerardo Cedillo-Servin,Ouafa Dahri,João Meneses,Joost van Duijn,Harrison Moon,Fanny Sage,Joana Silva,André Pereira,Fernão D. Magalhães,Jos Malda
3D Printed Magneto-Active Microfiber Scaffolds for Remote Stimulation and Guided Organization of 3D In Vitro Skeletal Muscle Models
Small (2024) -
Martina Viola,Madison J Ainsworth,Marko Mihajlovic,Gerardo Cedillo-Servin,Mies J van Steenbergen,Mattie van Rijen,Mylène de Ruijter,Miguel Castilho,Jos Malda,Tina Vermonden
Covalent Grafting of Functionalized MEW Fibers to Silk Fibroin Hydrogels to Obtain Reinforced Tissue Engineered Constructs
Biomacromolecules (2024)
Student opportunities
The Orthopaedic Biomechanics group provides courses and projects in the bachelor's and master's program.
Contact
-
Visiting address
Building 15, Gemini-South (room 4.115)Groene Loper5612 AZ EindhovenNetherlands -
Visiting address
Building 15, Gemini-South (room 4.115)Groene Loper5612 AZ EindhovenNetherlands -
Postal address
Department of Biomedical EngineeringP.O. Box 5135600 MB EindhovenNetherlands -
Postal address
Department of Biomedical EngineeringP.O. Box 5135600 MB EindhovenNetherlands -
Secretary
-
Teamlead
![[Translate to English:] Mahault Albarracin](https://assets.w3.tue.nl/w/fileadmin/_processed_/5/8/csm_Mahault%20Albarracin_0080904917.jpg)



![[Translate to English:] [Translate to English:]](https://assets.w3.tue.nl/w/fileadmin/_processed_/b/2/csm_Inloopspreekuur%20Algemeen_3a84590696.jpg)






