Improving a non-invasive way to monitor contractions during labor
Kirsten Thijssen defended her PhD thesis at the Department of Electrical Engineering on February 22nd. Her research was completed at Máxima Medical Center and Eindhoven University of Technology.

Uterine contractions are a key part of childbirth, but they can temporarily reduce oxygen supply to the fetus. During high-risk childbirth, monitoring of contractions is crucial to ensure safety for mother and unborn child. However, traditional monitoring techniques can be affected by maternal movements, or they are quite invasive. For her PhD thesis, Kirsten Thijssen measured the electrical activity from the uterus using non-invasive electrohysterography and considered its technological development and clinical implementation moving forward.
Uterine activity (UA) is usually monitored using a technique known as external tocodynamometry (TOCO). This is effectively a pressure sensor that is placed over the area with the strongest contractions, and it measures contraction frequency. However, accuracy is affected by the movements of the mother and obesity.
An alternative monitoring approach is an intra-uterine pressure catheter (IUPC) to measure contraction strength. However, IUPC is invasive and unpleasant for the mother. There are also risks associated with it, such as increased chances of bleeding and the potential requirement for a blood transfusion.
Due to these drawbacks with IUPC, suboptimal monitoring using TOCO has been the norm for decades, and the importance of UA monitoring has been overlooked in clinical practice.

Enter EHG!
To address the issues with other monitoring techniques, electrohysterography (EHG) is a promising non-invasive alternative. In EHG, a sensor is placed on the mother’s stomach where it measures electrical activity from the contracting uterus. The EHG method is based on prototypes developed by Eindhoven University of Technology in collaboration with Máxima MC.
“While such technologies are promising, it can take too much time for innovations to be put into clinical practice,” says Kirsten Thijssen, PhD researcher with the Department of Electrical Engineering at TU/e and Eindhoven MedTech Innovation Center.
For her thesis, Thijssen looked at ways to improve the development and clinical implementation of EHG as a new way to monitor UA.
First check with EHG
First, Thijssen conducted a validation study in which laboring women were simultaneously monitored with EHG and TOCO. The technique IUPC was used for reference measurements.
“EHG demonstrated significantly higher sensitivity to uterine contractions in comparison to TOCO,” says Thijssen. “Importantly, the accuracy of EHG remained unaffected by obesity, whereas the sensitivity of TOCO decreased.”

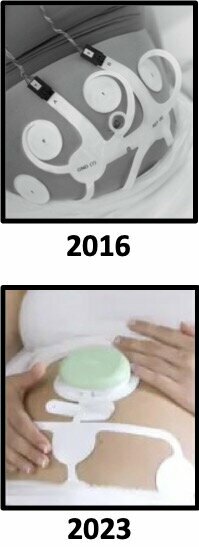
(Figure on right: Evolution of product design for electrophysiologic measurements during labor. 2007 - Bart van Overbeeke/Maastricht instruments; 2011, 2013, and 2023 - Nemo Healthcare; 2016 - Claudia Broekhoff)
To identify potential barriers and facilitators for implementation of the technology, patient and user perspectives were evaluated.
“Most patients preferred EHG over TOCO, but the healthcare professionals’ preferences were not as clear,” says Thijssen. “They offered recommendations for technology improvements, such as integrating an impedance meter and ensuring wireless and waterproof capabilities, which we embraced.”
China in your hands
Following the clinical validation, Thijssen and her collaborators then introduced EHG as a standard alternative for UA monitoring at Máxima MC for specific medical instances, such as obesity, previous cesarean sections, or poor results with TOCO.
“Comparative analysis with a group of women in which only TOCO was used showed no significant differences in childbirth outcomes, confirming the safety of EHG,” notes Thijssen.
To explore the impact of EHG in other clinical settings, Thijssen travelled to China to conduct a comparison of EHG and TOCO as a monitoring method for women opting to deliver their baby naturally after cesarean section (trial of labor after cesarean section or TOLAC) – with EHG providing a safe alternative for women who have had a cesarean section in the past.
“Since the abandonment of the one-child policy in China, most obstetricians were not yet familiar with a TOLAC,” says Thijssen. “In this trial, EHG-based uterine monitoring contributed to a safe and successful introduction of TOLAC in a Chinese hospital, resulting in a lower overall cesarean delivery rate.”
Both methods seemed to lower overall cesarean sections performed, while being equally safe.
Implementation in Europe
Thijssen’s research shows that UA monitoring with EHG is more accurate than with TOCO, both in obese and non-obese women, while still resulting in similar birth results.
“EHG is safe to be tested for other purposes in hospitals,” says Thijssen. “Our studies provide recommendations for small adaptations in technology development, future research, and learnings for successful implementation.”
In 2023, the improved wireless and waterproof system combining EHG with maternal and fetal electrocardiogram (ECG) was introduced. Currently, this system is being implemented across Europe for both intra- and extra-mural applications in obstetric care.
Hopes for the future
And when it comes to the future of EHG in healthcare, Thijssen has one clear desire: “I hope that there will be broad implementation of EHG. And I hope that my research can lead to more awareness about the importance of uterine activity monitoring in childbirth. UA deserves lots of attention, particularly during high-risk deliveries.”
But Thijssen is quick to point out that it can take decades before an innovation becomes commonplace in hospitals. “On average, it takes 17 to 20 years before a new technology makes an impact on broader clinical care. And less than half of all technologies make it to general use. Its impact on mothers and newborns alike must be properly evaluated.”
Besides monitoring uterine activity, Thijssen also foresees other applications for the technology. “It could be used in the diagnosis of preterm birth also, for instance.”
Title of PhD-thesis: Toward implementation of electrohysterography in clinical practice. Supervisors: S.G. Oei (TU/e), Beatrijs van der Hout-van der Jagt, and Michelle Westerhuis.
Other research partners: Máxima MC and Eindhoven MedTech Innovation Center (e/MTIC).
Media contact
Latest news


![[Translate to English:] [Translate to English:]](https://assets.w3.tue.nl/w/fileadmin/_processed_/e/0/csm_BvOF%202019_1031_BHF%20license%20TUe%20ILI%20copy_8a50884392.jpg)