Introduction
Currently, osteoarthritis is one of the most common diseases worldwide with a prevalence of 1 in every 10 adults. Osteoarthritis is believed to be initiated by mechanical overloading of cartilage and mainly occurs in the knee joint. Initiation of this full-joint disease can be accelerated by the presence of focal cartilage defects, which are characterized by well-defined locations on the articulating surface where cartilage has (partly) disappeared. Biological treatments such as debridement and autologous chondrocyte implantation have already shown promising results as a remedy for focal cartilage defects, yet they are only effective in patients less than 35 years old. Total knee arthroplasty could also function as a satisfying treatment for severe cases of joint diseases, but is only favorable for elderly since revision surgery is needed every 10-15 years while the surgical procedure becomes more complex every time. Thus, a gap of suitable treatments exists for patients between 35 and 65 years old. Cartilage resurfacing implants, which are metal implants that resurface the damaged location in the knee joint, may be a promising treatment for this age group. In general, two types of cartilage resurfacing implants are currently clinically used: a patient-specific implant, which perfectly aligns with the curvatures of the articulating surfaces in the knee joint, but is quite expensive and an implant with a generalized surface curvature, which matches the local curvature less well, but is less costly. However, the actual effect of implant curvature on the opposing and adjacent cartilage has not been studied, and is therefore the goal of this thesis.
Methods
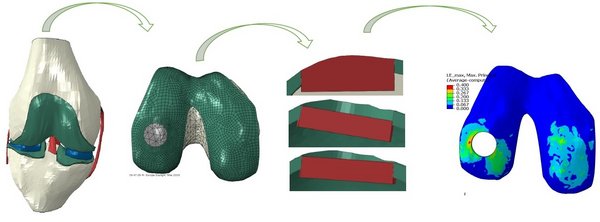
An open-source finite-element model of the knee was obtained and adjusted so that the stance phase of a gait cycle could be simulated. Rotations and translations were implemented as boundary conditions, while a force was applied to the knee joint in order to simulate axial loading during gait. Subsequently, cartilage resurfacing implants with different curvatures were placed in the femoral condyle to determine the effect of a curvature mismatch on the opposing and adjacent cartilage. Mechanical responses of cartilage to different implant curvatures were determined and related to biological events such as collagen fiber breakage, extracellular matrix damage and chondrocyte apoptosis. These outcomes were then analyzed in order to determine potential in vivo effects of different implant curvatures on cartilage.
Results
In general, implant-opposing tibial cartilage was affected more by implants with a surface close to the opposing cartilage than by implants with a surface that had less contact with the opposing cartilage. However, the highest strain values in tibial cartilage were usually caused by puncturing of the sharp implant edge into the tissue. Implant-adjacent femoral cartilage was mainly affected when implants were placed too deep into the cartilage, which caused the tissue to bulge over the edge of an implant, while the actual implant curvature did not seem to affect femoral cartilage. In most cases, a completely flat implant that was placed in the best possible way functioned comparable to perfect, patient-specific, implants and almost no effect of a mismatch in surface curvature was observed.
Discussion and Conclusion
It was found that implant-adjacent femoral cartilage was affected significantly more by flat implants with a bad placement than by perfect implants or flat implants with the best possible placement. Furthermore, the opposing cartilage was affected by perfect implants in the same way as by flat implants with a good placement. However, due to shortcomings of the cartilage model that was used in the current study, it was not possible to actually predict cartilage damage based on biological thresholds. Based on the results of this study, it is proposed that cartilage resurfacing implants with a generalized curvature should be used over a patient-specific implant, as they are associated with less costs but similar functionality.